Medical innovation-2022
5. Da Vinci surgery-The da Vinci surgical system gives your surgeon an advanced set of instruments to use in performing robotic-assisted minimally invasive surgery. The term “robotic” often misleads people. Robots don’t perform surgery. Your surgeon performs surgery with da Vinci by using instruments that he or she guides via a console.
- In the U.S., the da Vinci SP system is only cleared for use in single-port urological procedures, lateral oropharyngectomy procedures (commonly referred to as radical tonsillectomy) and tongue base resection.
In 2000, the da Vinci Surgical System became the first robotic surgical platform commercially available in the United States to be cleared by the FDA for use in general laparoscopic surgery. There are more than 1,700 da Vinci Systems installed in hospitals worldwide.
6. Result of using NO donators at surgical treatment of ekzofit forms of papilomaviridae issues of anorectal regions-criodistructions
Papillomaviridae is a family of non-enveloped DNA viruses whose members are known as papillomaviruses.[1] Several hundred species of papillomaviruses, traditionally referred to as "types",[2] have been identified infecting all carefully inspected mammals,[2] but also other vertebrates such as birds, snakes, turtles and fish.[3][4][5] Infection by most papillomavirus types, depending on the type, is either asymptomatic (e.g. most Beta-PVs) or causes small benign tumors, known as papillomas or warts (e.g. human papillomavirus 1, HPV6 or HPV11). Papillomas caused by some types, however, such as human papillomaviruses 16 and 18, carry a risk of becoming cancerous.[6]
Papillomaviruses are usually considered as highly host- and tissue-tropic and are thought to rarely be transmitted between species.[7] Papillomaviruses replicate exclusively in the basal layer of the body surface tissues. All known papillomavirus types infect a particular body surface,[2] typically the skin or mucosal epithelium of the genitals, anus, mouth, or airways.[8] For example, human papillomavirus (HPV) type 1 tends to infect the soles of the feet, and HPV type 2 the palms of the hands, where they may cause warts. Additionally, there are descriptions of the presence of papillomavirus DNA in the blood and in the peripheral blood mononuclear cells.
Papillomaviruses were first identified in the early 20th century when it was shown that skin warts, or papillomas, could be transmitted between individuals by a filterable infectious agent. In 1935 Francis Peyton Rous, who had previously demonstrated the existence of a cancer-causing sarcoma virus in chickens, went on to show that papillomavirus could cause skin cancer in infected rabbits. This was the first demonstration that a virus could cause cancer in mammals.
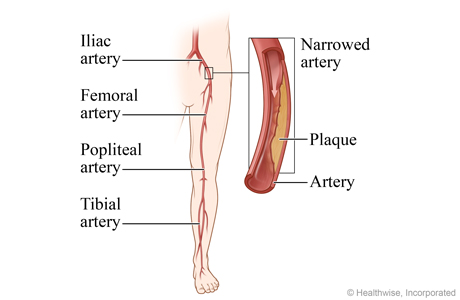
7.ERAS protocol-Enhanced recovery after surgery (ERAS) protocols are multimodal perioperative care pathways designed to achieve early recovery after surgical procedures by maintaining preoperative organ function and reducing the profound stress response following surgery.8. Leriche's syndrome is the term used for a group of symptoms that are caused by a certain type of peripheral arterial disease of the legs. In Leriche's syndrome, blood flow in the aorta is blocked in the stomach area. This blocks blood flow to the legs. In men, blood flow to the penis is also blocked.
The following symptoms happen:
- Leg weakness or numbness.
- Pain in the thighs, hips, and buttocks (intermittent claudication).
- Erectile dysfunction (impotence).
- Weak pulse in the thigh arteries (femoral arteries).
Treatment for PAD includes ways to relieve symptoms and lower your risk of heart attack and stroke. Healthy lifestyle changes and medicines can help relieve symptoms and lower this risk. In some cases, you may need surgery or a procedure called angioplasty.
When you have PAD, you have a high risk of having a heart attack or stroke. Making healthy changes along with taking medicines can help reduce this risk.
Lifestyle changes
- If you smoke, quit. It's one of the most important things you can do. If you need help, talk to your doctor about programs and medicines that can help you stop.
- Eat healthy foods.
- Get regular exercise (if your doctor says it's safe). Try walking, swimming, or biking for at least 30 minutes on most, if not all, days of the week. If you have symptoms when you exercise, your doctor might recommend a specialized exercise program that might relieve your symptoms.
- Manage your cholesterol and blood pressure if they are high. You may need medicines to help you do this.
- If you have diabetes, keep your blood sugar in a target range.
- Lose weight if you need to, and maintain a healthy weight.
- Take good care of your feet and legs. When you have reduced blood flow to your legs, even minor injuries can lead to serious infections.
Your doctor may suggest that you attend a cardiac rehabilitation (rehab) program. In cardiac rehab, you will get education and support to help you make new, healthy habits.
Medicines and surgery
You may take medicine to lower your risk of heart attack and stroke. These medicines help prevent blood clots, manage blood pressure, and manage cholesterol.
If lifestyle changes don't help relieve symptoms, your doctor may prescribe a medicine that may relieve the pain when you walk.
If you have symptoms that make it hard for you to walk, you might choose to have a procedure called angioplasty or bypass surgery. These treatments open narrowed arteries or reroute blood flow around them. Angioplasty or surgery might also be done if blood flow to your leg is severely limited.
In rare cases, advanced PAD can cause tissues in the leg or foot to die because they don't get enough oxygen as a result of poor blood flow. If this happens, part of the leg or foot must be removed (amputated). This is more common in people who also have diabetes.
Leriche syndrome, also known as aortoiliac occlusive disease, is characterized by the blockage of the abdominal aorta as it transitions into the common iliac arteries. Leriche syndrome is considered a form of peripheral artery disease, as it is characterized by a narrowing of the arteries other than those that supply the heart or the brain.
The abdominal aorta is the largest artery in the abdominal cavity and supplies blood to many of our vital internal organs and other tissue via its many branches. The common iliac arteries are comprised of two large branches and many diverging branches to provide blood to the pelvis and lower limb.
Causes of Leriche syndrome
The primary cause of Leriche syndrome is an atherosclerotic disease of the aorta. This is a condition of the arteries that make them become narrower due to plaque buildup. Atherosclerosis is considered a condition that affects older individuals as it takes years for a big enough plaque to develop. Arterial plaque is typically made up of calcium, fat, cholesterol, and other substances found in your blood. Atherosclerosis can also cause arteries to become stiff, causing restricted blood flow.
Other possible causes of Leriche syndrome include:
- Takayasu’s arteritis – an inflammatory condition in the arteries that can cause blockage
- Radiation to the pelvis – can cause progressive inflammation in the arterial wall leading to blockage
- Thrombosis
- Emboli
- Congenital diseases – includes aplasia and hypoplasia
Symptoms of Leriche syndrome
Leriche syndrome symptoms vary depending on the degree of vessel occlusion, with some patients not showing any symptoms at all. However, since the abdominal aorta and its many branches supply oxygenated blood to many important structures, symptoms will be apparent when they do present themselves. Often times, patients with Leriche syndrome will have intermittent symptoms that resolve soon after they develop. These symptoms can include:
- Fatigue of both lower limbs
- Leg weakness or numbness
- Muscle cramping pain in the thigh, hips, and buttocks (intermittent claudication)
- Erectile difficulty in men
- Weak pulse in femoral arteries
- Cold and pale extremities
- Ulcers on lower leg
- Gangrene of the toes and lower leg
The condition will often first manifest itself as not being able to walk for long distances, with even short distances becoming a challenge. Patients may then start to notice that the skin on their legs and feet begin to appear drier and scaly. A loss of lower leg hair may also be seen due to poor blood supply. Later stages of Leriche syndrome tend to be destructive, as toes begin to hurt and pain becomes more permanent. If Leriche syndrome treatment is not sought out right away at this point, significant cell damage and death may occur.
Diagnosis of Leriche syndrome
Diagnosis will often begin with a detailed description of your past medical history and currently presenting symptoms. This is to allow the doctor to differentiate between several other causes that may present in a similar fashion. Next, a physical exam will take place, which will allow the doctor to evaluate the condition of the affected skin, muscle mass, and temperature of the extremities. Documenting the pulses of the lower extremities is also very important for peripheral artery diseases such as this. Pulse areas that are checked include the radial, brachial, femoral, and popliteal.
Once a suspected diagnosis of Leriche syndrome has been made, more accurate diagnostic testing will be in order. Initially, testing will include taking an ankle-brachial index and a duplex ultrasound. These tests will give a good first evaluation that can be confirmed using more accurate testing.
Further testing often includes imaging tests using computed tomography (CT) angiography, which combines an injection of contrast media and the imaging scan to get a better look at the vessels of the body. CT angiography is a great test to visualize and assess the site of occlusion and stenosis. A magnetic resonance angiography (MRA) may be substituted if a CT is not possible.
Treatment for Leriche syndrome
Correcting and restoring blood supply to affected areas by enhancing vascularization is the goal of treatment in Leriche syndrome. This may take many forms:
- Treating underlying risk factors: Treating pre-existing conditions such as hyperlipidemia, diabetes, and hypertension and keeping them under control will help reduce the chances of developing peripheral artery disease. Staying healthy by eating a balanced diet and quitting bad habits such as smoking cigarettes will also help to reduce the chances of developing atherosclerosis.
- Supportive treatment: Involves staying active and performing various exercises that aim to boost the use of oxygen by muscles in the lower extremities. This may include walking, running, or other exercises that involve the legs.
- Medical intervention: If none of the previously mentioned treatments have proven successful, the use of drugs to relieve claudication may be recommended. Pentoxifylline and Cilostazol are two commonly used drugs in the treatment of peripheral artery disease. Medications to reduce clotting may also be implemented depending on the circumstance
- Surgical intervention: May involve procedures such as aortoiliac endarterectomy, percutaneous transluminal angioplasty with or without stent placement, aorto-bifemoral bypass, axillary-bi-femoral and femoral-femoral bypass. These procedures aim to either remove the occasion or create a bypass around it.
Prevention of Leriche syndrome
The best way to prevent the development of Leriche syndrome is to not expose yourself to the risk factors that cause it in the first place. This will require you to stop smoking and manage chronic underlying conditions such as diabetes, cholesterol, and high blood pressure.
It is also recommended to eat a healthy well-balanced diet that is low in fat and cholesterol while getting regular exercise.



Коментарі
Дописати коментар